Use of the Gait Profile Score for the evaluation of patients with joint hypermobility syndrome/Ehlers-Danlos syndrome hypermobility type.
Abstract:
Gait analysis (GA) is widely used for clinical evaluations in various pathological states, both in children and in adults, such as in patients with joint hypermobility syndrome/Ehlers-Danlos syndrome hypermobility type (JHS/EDS-HT). Otherwise, GA produces a large volume of data and there is the clinical need to provide also a quantitative measure of the patient's overall gait. Starting from this aim some global indexes were proposed by literature as a summary measure of the patient's gait, such as the Gait Profile Score (GPS). While validity of the GPS was demonstrated for the evaluation of the functional limitation of children with Cerebral Palsy, no studies have been conducted in patients JHS/EDS-HT. The aim of our study was therefore to investigate the effectiveness of the GPS in the quantification of functional limitation of patients with JHS/EDS-HT. Twenty-one adult (age: 36.1±12.7 years) individuals with JHS/EDS-HT were evaluated using GA and from GA data the GPS was computed. The results evidenced that the GPS value of patients was 8.9±2.6, statistically different from 4.6±0.9 displayed by the control group. In particular, all values of Gait Variable Scores (GVS) which compose the GPS were higher if compared to controls, with the exception of Pelvic Tilt and Foot Progression. The correlations between GPS/GVS and Lower Extremity Functional Scale (LEFS) showed significant relationship between GPS and the item 11 ("Walking 2 blocks") (ρ=-0.56; p<0.05) and 12 ("Walking a mile") of LEFS (ρ=-0.76; p<0.05). Our results showed that GPS and GVS seem to be appropriate outcome measures for the evaluation of the functional limitation during gait of patients with JHS/EDS-HT.PubMed info here.
 I hate cancelling plans. I absolutely despise having to make the call (or send an email) in order to let someone down. It makes me feel like a huge disappointment of a person. My other choice is to simply not make plans at all, but then I begin to feel like a hermit. If I have something on my schedule, that means I'm not turning into a recluse, right?
I find myself in the cancelling conundrum all too often. My close friends and family know of my condition, although some do not know of the extent of my disability. How to tell them why I need to cancel without scaring them? Or making them feel like they need to visit and take care of me? Being honest is important, but sometimes I don't want to reveal all of my personal information (TMI much?). I also don't want to trivialize what is happening. I feel like I'm am constantly doing a delicate balancing act to keep people informed, yet protected. And that state of being is lonely.
My balancing act applies not only with the making and breaking of plans; I do this for all aspects of sharing my life with EDS. I will always tell people enough so that our relationship can function; however, I keep much of what I'm going through to myself. Even my husband does not know 100%--I will always withhold some information. I do this in order to protect him and his mental state (he really doesn't need to know how many times things dislocated today) and to keep my independence (if he did know everything, he would be afraid to let me do anything).
This balancing act probably sounds insane to the majority of people. But, I expect for those with chronic illness, it will sound familiar. I would love to hear your thoughts in the comments.
Belgium doctors researching ACL tears found a previously unknown ligament, the anterolateral ligament (ALL), in human knees. Article here.
 I know there are people out there whose sleep is described as being so deep "the house could fall down, and s/he wouldn't wake up." I am not one of those people. Every little noise can, and will, wake me. Of course, once I'm awake, I will realize I'm uncomfortable and spend the next 20 minutes trying find a new sleeping position that won't hurt or threaten to dislocate anything.
I've found that white noise will prevent at least one source of awakening. When I'm at home, I usually rely on my trusty desktop (here, nightstand) fan. However, whenever I have to be away from home, I make sure to have my iPad just for a white noise app. My favorite by far (and free!) is Relax M. HD. It is available for Apple products and for Android. There is an upgraded version of this app as well, but I've been happy with the free basic version. The reason I prefer this app is that it gives you a number of "base" white noises, which are fine on their own, or you can combine each "base" noise with another to create a more complex and rhythmic white noise. A free product that will help me to get a better night's sleep? Definitely EDSer recommended!
Pregnancy and delivery in ehlers-danlos syndrome (hypermobility type): review of the literature.
AbstractEhlers-Danlos syndrome (EDS) is a group of connective tissue disorders which are divided into various distinguishable phenotypes. The type of EDS determines the potential obstetric complications. Due to the spectrum of clinical manifestation and overlap between phenotypes, there are no standardised obstetric management guidelines. Existing literature illustrates different obstetric management in hypermobility type of EDS, including uneventful term vaginal deliveries as well as preterm cesarean section deliveries. This paper discusses obstetric management of a woman with EDShypermobility type. Cesarean section was deemed the most appropriate delivery method in this patient due to the possible complications including risk of joint dislocation and pain morbidity. No obstetric complications were experienced, and good maternal and neonatal outcomes were achieved.
Full text here.
 There are days (like today--another rainy, damp, icky one) where it is hard to separate myself and my EDS. My EDS is so intertwined with everything about me: how I feel, how I act, how I move. It's hard to remember that EDS is NOT me. Of course, it's become a part of my life, a much larger part than I ever would have imagined. However, facing pain and disability has also forced me to grow as a person--to become stronger, more observant, more flexible, more patient. I've slowed down a lot, but I've gained a perspective on life that I was never allowed before, always rushing from place to place. EDS has, of course, changed me. But it is not me.
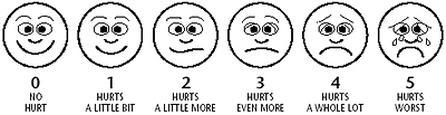
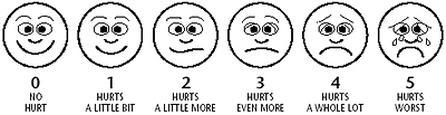 I bet you are sick and tired of hearing "on a scale of 1-10, how bad does ____ hurt?" ("Well, on my personal scale, or yours? 'Cause a 3 for me is like a 7 for normal people. And do you want a number just for ___ or for overall? What about other body parts that hurt now, too? And for good days or bad days?") Or trying to draw where things hurt on a body outline? ("May I just scribble over the whole freakin' thing?") I found this fantastic post awhile ago by one of my favorite bloggers, Allie Brosh. It made me laugh so hard, I popped a few ribs in the process. So brace yourselves (and your rib cage) for the new pain scale.
Evaluation of Kinesiophobia and Its Correlations with Pain and Fatigue in Joint Hypermobility Syndrome/Ehlers-Danlos Syndrome Hypermobility TypeAbstract:Ehlers-Danlos syndrome hypermobility type a. k. a. joint hypermobility syndrome (JHS/EDS-HT) is a hereditary musculoskeletal disorder associating generalized joint hypermobility with chronic pain. Anecdotal reports suggest a prominent role for kinesiophobia in disease manifestations, but no study has systematically addressed this point. Objective. To investigate the impact of kinesiophobia and its relationship with pain, fatigue, and quality of life in JHS/EDS-HT. Design. Cross-sectional study. Subjects/Patients. 42 patients (40 female and 2 male) with JHS/EDS-HT diagnosis following standardized diagnostic criteria were selected. Methods. Disease features were analyzed by means of specific questionnaires and scales evaluating kinesiophobia, pain, fatigue, and quality of life. The relationships among variables were investigated using the Spearman bivariate analysis. Results. Kinesiophobia resulted predominantly in the patients' sample. The values of kinesiophobia did not correlate with intensity of pain, quality of life, and (or) the single component of fatigue. A strong correlation was discovered between kinesiophobia and general severity of fatigue. Conclusions. In JHS/EDS-HT, the onset of pain-avoiding strategies is related to the presence of pain but not to its intensity. The clear-cut correlation between kinesiophobia and severity of fatigue suggests a direct link between musculoskeletal pain and fatigue. In JHS/EDS-HT, the underlying mechanism is likely to be facilitated by primary disease characteristics, including hypotonia.Full article here.
 I tend to pick on physicians a bit. I think it is something that all of us with a "rare" illness do to keep ourselves sane. I will say, there are some good docs out there. I have had the good luck in finding a few myself. However, oh boy, are there some baaaaaaad ones. The ones that tell you that your dislocations are "all in your head." (But...ummm...my shoulder is hanging out of it's socket?) The ones that tell you, if you come prepared with articles, etc., that you are Google-diagnosing yourself, and you MUST be a hypochondriac. I could go on and on. But here is the good news. At the Greater Baltimore Medical Center, an EDS Center will be opening soon! This center will focus on physician education as well as patient care. Find out more here.
 Note to self, and to you, dear reader: please remember this today, and every day. Those of us with chronic illness (especially when chronic pain is involved) tend to be extremely hard on ourselves. I know I am. I hate it when I don't get through my to-do list (or, some days, even look at it). I start that vicious cycle of thinking "I could have done this easily before I was sick! And a lot more! On 4 hours of sleep! Etc., etc." And what does that accomplish, (well, other than making me feel horrible, guilty, and lazy)? Absolutely nothing. So, this is my new mantra to repeat to myself when I feel the bad thought cycle starting: "I love you, you did the best you could today, and even if you didn't accomplish all you had planned, I love you anyway." It is time to let go of the guilt.
|

 RSS Feed
RSS Feed