Impairment and impact of pain in female patients with Ehlers-Danlos syndrome: a comparative study with fibromyalgia and rheumatoid arthritis.
Abstract:Objective: The purpose of this study was to investigate functional impairment and the impact of pain in patients with Ehlers-Danlos syndrome, hypermobility type (EDS-HT), and to compare the burden of disease with that in women with fibromyalgia (FM) and rheumatoid arthritis (RA).
Results: The study results showed clinically relevant health-related dysfunction in all groups. Significantly poorer physical, psychosocial, and overall function was found in the EDS-HT group compared with the RA group. In comparison with the FM group, the EDS-HT group reported similar physical and overall function, but better psychosocial function. T scores from the MPI revealed significantly higher levels of pain severity and life interference due to pain, and a lower level of perceived life control, in the EDS-HT group compared to the RA group. In contrast, the EDS-HT group showed significantly lower levels of pain severity, life interference, and affective distress in comparison with the FM group. Social support for help in coping with pain was similar between the 3 groups.
Conclusion: EDS-HT is associated with a consistent burden of disease, similar to that of FM and worse than that of RA, as well as a broad impact of chronic pain on daily life, which needs to be addressed in the health care system.Full text here.
 I spend hours on the phone each week fighting with people in order to coordinate and pay for my care. By "people" I mean the poor souls who have the answer the customer line at my insurance company, and my doctors' offices, and the place that takes my blood, and the hospital, and the testing facility...the list goes on. And by "fighting", I mean that I'm too nice, so I really spend hours on the phone each week politely explaining my case to try to make people care about my plight and then do their jobs.
Sometimes my problem is resolved with a phone call. However, usually it drags on and on--multiple long calls are needed, sometimes letters need to be drafted and sent, I even have made personal visits to billing offices to clear up issues (I'm sure they loved that). I noticed that the reason my problems take months to be solved is that they get passed from office to office. No one wants to deal with a problem, especially when I might just give up and pay them. This summer, I had a few x-rays done of my neck by order of one of my physicians. I got the x-rays at the same hospitals where that physician practices. Both the hospitals and the physician were covered by my insurance; however, my insurance refused payment because my "preventative schedule" did not cover the x-rays. I discovered (after calls to my insurance) that the x-rays should have been billed at diagnostic, not preventative. Somewhere along the way, the billing code was incorrectly changed. After approximately 3 dozen calls to the various parties, I still don't know how the mistake was made or who made it, but it was mysteriously fixed and my insurance paid.
I think billing and insurance issues happens to those with chronic illnesses on a regular basis. Mainly because we require more care, but I also sometimes wonder if a handful of others try to take advantage of us. I believe there is always that chance when an ill or disadvantaged individual is involved. My advice to you is to always double check you EOBs and bills: do they match? Also, actually read your EOBs and check the codes at the bottom. Is your insurance covering all that it should be covering? If there is an odd code, don't hesitate to call your insurance to ask about it. Also, find out if your doctor can re-write a prescription/order so that it can be covered. If you are having a problem with your doctor's office, speak to the billing department, and don't be afraid to ask for the office manager.
Dysphagia in patients with the joint hypermobility syndrome
Abstract:Results: 17 patients with JHS and dysphagia were referred by the rheumatologists to our unit in 1 year: 76% female; age range: 12–58. None had evidence of a structural cause for the dysphagia on either gastroscopy or barium studies. 10 (59%) had an oesophageal dysmotility to account for their dysphagia – out of these one had achalasia; the other 9 (53%) had oesophageal hypomotility with 7 having frequent hypotensive peristalsis and 2 having intermittent hypotensive peristalsis. 33% of those with hypomotility had a normal Multiple Rapid Swallow test (MRS). 7 of the 17 patients (41%) had normal oesophageal motility and 6 of these had reflux studies: 50% had GOR, 17% had a hypersensitive oesophagus and the remaining 33% had normal studies. Only 2 patients (12%) had hiatus hernias and both of these had oesophageal hypomotility and no GOR.
Conclusion: This is the first study of upper GI physiology in patients with JHS and non-structural dysphagia. Oesophageal hypomotility is common in these patients and those patients with normal MRS are likely to show the best response to prokinetics. 50% of those with normal motility had pathological GOR and would benefit from high dose proton pump inhibitor therapy. The remainder had normal studies, suggesting hypersensitivity which may respond to treatment with neuromodulators such as amitriptyline. Only 12% of patients had a hiatus hernia, which is in contrast to previous studies.3 Further prospective studies are required to understand the pathophysiology and management options for dysphagia in JHS.Text here.
 In the blink of an eye, you life can change due to a diagnosis of a chronic, incurable disorder. You are forced to come to a screeching halt before taking a sharp turn. Your goals, dreams, and priorities must change. You may grieve and feel the loss of your former self; however, you become grateful for the little things in life--the things that seemed too trivial to notice previously . Worrying about life's minutiae suddenly takes up less of your time. You must now determine how to use each and every ounce of energy, and make it count. Your energy must be spent on people and things that are meaningful to you. Needless drama is cut out of your life. This new life can be confining in ways, but also liberating. Live it.
 This is me today. This is me on most days, actually, but my brain fog seems to be especially bad today. "Fog" is a good description for it; I feel like I'm wandering through a rain forest shrouded in thick fog when I'm attempting to figure out the word I want or what I'm doing on Saturday. The cognitive problems are actually the part of EDS I hate the most. I feel that if the disorder took over my body, it should very well leave my brain alone? Apparently not the case, however. So I am left chugging along, slowly, through the fog.
Management of pain and fatigue in the joint hypermobility syndrome (a.k.a. Ehlers-Danlos syndrome, hypermobility type): principles and proposal for a multidisciplinary approach.Abstract:Joint hypermobility syndrome (JHS), or Ehlers-Danlos syndrome (EDS) hypermobility type (EDS-HT), is a underdiagnosed heritable connective tissue disorder characterized by generalized joint hypermobility and a wide range of visceral, pelvic, neurologic, and cognitive dysfunctions. Deterioration of quality of life is mainly associated with pain and fatigue. Except for the recognized effectiveness of physiotherapy for some musculoskeletal features, there are no standardized guidelines for the assessment and treatment of pain and fatigue. In this work, a practical classification of pain presentations and factors contributing in generating painful sensations in JHS/EDS-HT is proposed. Pain can be topographically classified in articular limb (acute/subacute and chronic), muscular limb (myofascial and fibromyalgia), neuropathic limb, back/neck, abdominal and pelvic pain, and headache. For selected forms of pain, specific predisposing characteristics are outlined. Fatigue appears as the result of multiple factors, including muscle weakness, respiratory insufficiency, unrefreshing sleep, dysautonomia, intestinal malabsorption, reactive depression/anxiety, and excessive use of analgesics. A set of lifestyle recommendations to instruct patients as well as specific investigations aimed at characterizing pain and fatigue are identified. Available treatment options are discussed in the set of a structured multidisciplinary approach based on reliable outcome tools.
Full article here.
 I love to cook. I have been cooking for my family and my friends since I was about 12. Of course, my dishes have gotten vastly more complex since the days where my parents were still a little nervous that I would burn the house down. (As a side note: I have come close to doing so recently with my memory lapses. My husband now double checks that the burners are off. This is always a good suggestion if you suffer from brain fog.) However, though I want to make fun, yummy, and allergy-free meals, the EDS pain can interfere with my plans. Over the past few years, I have come across some kitchen implements that I have found make working in the kitchen much, much easier, whether for executing a complicated recipe or for making a quick, no-fuss dinner. In no particular order:- Stand mixer. I have a KitchenAid stand mixer (a gift from my mom and sister), and I can definitively say it is worth the price. Anything I would otherwise have to stir--into the mixer it goes. The only downside is that it takes up a ton of counter space, so if you have to store it in a cabinet, be prepared to need a helping hand to get it out and in place on the counter.
- Microwavable steamer pot. Another gift from my mom. Mine is from Pampered Chef (I think my mom felt she had to buy something at a party). It is fantastic for steaming veggies and potatoes. You can make a side dish in minutes or prep something for the oven so it takes much less time to roast.
- Crock Pot. The old standby. I love slow-cooker recipes. I make a lot of soups and stews in mine. I also make turkey, chicken, casseroles, barbecue, etc. If you are making meat (e.g., a turkey tenderloin), make sure you put vegetables and/or fruit in with it to keep things moist and flavorful while cooking.
- Sharp knives. You hear about the virtues of these on all the cooking shows, but it really is true. It takes much less wrist energy to chop (and there's much less of a chance of cutting yourself) with a good, sharp knife.
- Large wok pan. You can make just about anything in this pan and the high sides prevent spills. I do "clean out the refrigerator" stir fry nights with some shrimp and, well, whatever happens to be in the fridge.
Do you have any suggestions for this list? If so, please add them in the comment
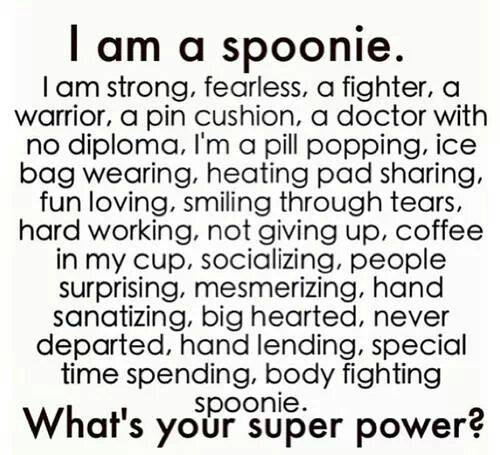
Not familiar with the spoon theory? Read about it here.
|



 RSS Feed
RSS Feed